Dysfunction of the temporomandibular joint (TMJ) in the jaw, such as stiffness, clicking, or muscle tension, can cause headaches or pain in the face, teeth, eyes, ears, and neck. When problematic, the joint can even interfere with proper functioning—such as chewing, biting, opening the mouth (even yawning), dislodging food stuck behind the teeth, or brushing your teeth easily. Physiotherapy treatment for the temporomandibular joint is an effective way to relieve this pain and restore normal jaw function.

What is the temporomandibular joint?
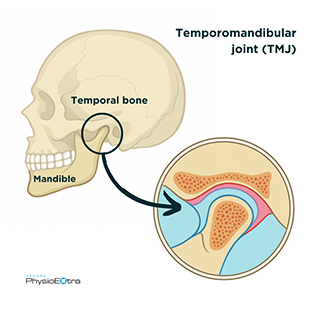 The jaw joint, called the temporomandibular joint (TMJ), is located on each side of the head, just in front of the ears. It connects the lower jawbone (the mandible) to the skull (the temporal bone).
The jaw joint, called the temporomandibular joint (TMJ), is located on each side of the head, just in front of the ears. It connects the lower jawbone (the mandible) to the skull (the temporal bone).
Like all joints, the TMJ is made up of cartilage on the articular surfaces, ligaments, muscles, tendons, and a fluid that helps lubricate it. It also contains a small articular disc (meniscus) that moves with the jaw. This disc helps stabilize the joint during movement and properly distributes pressure when chewing.
What causes jaw pain?
Jaw pain can be caused by a traumatic injury, such as:
- a blow to the jaw;
- a fall on the chin;
- a sudden opening/closing of the jaw in a car accident (also known as jawlash).
Such incidents can lead to inflammation and various jaw injuries such as a fracture, dislocation, sprain, or muscle spasm.
Jaw pain can also develop over time due to:
- poor lifestyle habits (e.g., constantly chewing gum, nail-biting, frequently biting lips, or regularly resting the chin in your hand);
- bruxism (clenching or grinding teeth);
- stress;
- poor posture maintained repetitively or for prolonged periods;
- poor dental occlusion, meaning the way your upper and lower teeth come together;
- dental procedures that require keeping the mouth wide open for several minutes;
- etc.
A combination of these factors can lead to muscle tension and contribute to jaw or neck pain, headaches, and sometimes ear-related symptoms such as pain, a feeling of fullness in the ear, or tinnitus (like ringing or buzzing in the ears).
How do you relieve jaw pain?
Temporomandibular joint (TMJ) in physiotherapy treatment
Physical therapists with advanced training in the treatment of the temporomandibular joint can assess and treat jaw pain. Treatments can take the form of manual therapy techniques, muscle relaxation, and exercises. You will also receive personalized advice on your posture, your lifestyle or activities to modify to reduce or even eliminate your jaw pain. Learn more about this expertise.
Book an appointment today at a clinic near you.
Frequently asked questions (FAQ)
Clenching or grinding your teeth? Bruxism
Bruxism refers to clenching or grinding your teeth, often during sleep. The jaw muscles are overworked when they should be at rest. Bruxism can cause jaw pain, especially when combined with stress, poor lifestyle habits, or bad posture. During periods of stress or intense concentration, some people even clench their teeth during the day. If that’s the case, it’s important for the person to become aware of the habit and correct it to avoid overloading the muscles. However, if bruxism is the only factor involved, it may sometimes cause no pain at all.
Since bruxism can wear down teeth more quickly, a dentist may recommend a night guard to protect them while sleeping. Combined with physiotherapy treatment, this approach can help reduce pain and protect the teeth. That’s why dentists and physiotherapists often work together in treating jaw pain.
Jaw tension or spasms? Muscle syndrome
Most people who consult a physiotherapist for jaw pain suffer from a muscle syndrome. This condition is caused by tension or spasms in the muscles of the jaw, neck, or face.
Muscle syndrome can appear suddenly (such as a muscle spasm following a dental procedure involving an anesthetic injection into the muscle, known as trismus). It can also develop over time due to bruxism, stress, poor posture, secondary issues in the neck, or certain lifestyle habits.
Jaw clicking or cracking?
Some people may notice a sound like a “click” or a crack when opening and/or closing the mouth. This sound can be constant or intermittent, occur on one or both sides of the jaw, and may or may not be accompanied by a deviation of the chin when opening. This condition is not necessarily associated with pain or limitations.
The cause of this sound is most often a displacement of the articular disc inside the temporomandibular joint. Sometimes, the disc slips slightly forward and makes a noise when you open your mouth, as it returns to its place beneath the condyle (the part of the mandible that articulates with the skull). If this noise is not accompanied by pain or functional difficulties (chewing, biting, speaking, or fully opening the mouth), there is generally no cause for concern.
Some people, however, may hear a louder noise, like a “clunk”, when opening their mouth very wide to yawn or eat. This sound is associated with a jaw subluxation, meaning the condyle of the mandible (the lower jawbone) slides too far forward and moves past the small bony prominence of the temporal bone. This can give the sensation that the jaw might get stuck, although it can still be closed. In some cases, the mouth may actually remain stuck open. It is possible to reposition it by pulling the mandible downward, but we strongly recommend seeking prompt medical attention in such a situation.
If you experience pain or if your jaw movements are impaired, be aware that physiotherapy treatment for the temporomandibular joint can help relieve your pain, stabilize the joint, and restore normal jaw function.
Jaw locking? Limited opening or closing
There are primarily two types of jaw locking: limited opening and limited closing.
Limited opening
If you are unable to open your mouth wide enough to bite into an apple or a hamburger, visit the dentist, sing, or even brush your teeth, this is referred to as a limitation in mouth opening. It can be caused by joint stiffness due to factors such as a muscle spasm, osteoarthritis, arthritis, capsulitis, or the disc not returning to its position. This type of locking can quickly become very disruptive in your daily life.
Limited closing
If, on the other hand, you are unable to close your mouth (a situation that can be quite distressing), this is referred to as a limitation in mouth closing. This issue is usually associated with a jaw dislocation following an accident. It may also be caused by an overly wide or prolonged mouth opening in people with ligament hyperlaxity, meaning excessive looseness of the ligaments that stabilize the joints—similar to the jaw subluxation mentioned earlier. If this is your case, an appointment with a dentist or a physiotherapist should be scheduled promptly to reposition the jaw.
What are the symptoms of osteoarthritis of the jaw?
Osteoarthritis is the wearing down of the cartilage that covers the ends of the bones in the jaw joint. It is a normal part of the aging process, also linked to genetic predispositions, and does not always cause symptoms. When symptoms do appear, the most common are stiffness and noises such as crackling or grinding sounds. These may sometimes be accompanied by pain, muscle tension, or weakness.
A history of jaw injuries or issues, as well as prolonged poor posture, can contribute to the early onset of osteoarthritis.
I had jaw surgery. Should I consult a professional?
There are several types of jaw surgeries. In most cases, the maxillofacial surgeon recommends and prescribes physiotherapy for TMJ rehabilitation after the procedure. Pain is not always the main concern—more often, it is limited mobility, stiffness, muscle weakness, and muscle tension that need to be addressed post-operatively.
In all cases, a thorough evaluation is necessary after surgery to improve jaw function (opening, chewing, dislodging food in the mouth, speaking, etc.), restore a better quality of life, prevent compensation by other joints (such as the neck), and eliminate pain if present.
When I open my mouth, I feel pain in my ear, is that normal?
It is possible for the jaw joint to cause ear pain. This is not only because of its close proximity to the ear, but also because certain muscles that are stretched when opening the mouth—such as the masseter—can radiate pain to the ear area.
When should you be concerned about jaw pain?
The jaw should not cause pain. That’s why it’s important to consult a professional promptly when pain appears, in order to avoid developing compensatory behaviors and allowing tension and stiffness to set in.
How can you relieve jaw pain?
Since jaw pain can stem from various causes and contributing factors, a physiotherapist or an osteopath will be able to properly assess your condition to identify the issues causing your pain and provide effective relief.
While waiting for your appointment, the first step is to only open your jaw within a pain-free range of motion, reduce the load on your jaw muscles by taking smaller bites, opt for foods that are not too hard to chew, and avoid using your jaw for non-essential activities (chewing gum, nail-biting, lip-biting, resting your chin in your hand).
Who should I consult if I have jaw pain?
Physiotherapists with advanced training in manual therapy or specific training in TMJ assessment and treatment can help address your condition. Osteopaths are also highly qualified healthcare professionals who can assist in resolving this issue.


